
A total hip replacement that incorporates patient-specific instrumentation and 3D technology is a surgical procedure that involves the use of advanced software and tools to help improve the accuracy and precision of your hip replacement. Specifically, this technology allows for pre-operative planning using 3D imaging and modelling of your anatomy and enables Dr Singh to create a personalised surgical plan that is matched to your unique anatomy.
During your procedure, patient-specific instrumentation is used to assist Dr Singh in accurately positioning the implant components. This instrument is designed specifically for you, ensuring that the implant is placed in the optimal position.
Dr Singh uses computer-assisted, patient-specific, and 3D technology in all his total hip replacement procedures because it provides a higher degree of precision and accuracy, which can result in improved outcomes and satisfaction for you as his patient.
In the lead up to your total hip replacement procedure, Dr Singh will carry out a complete physical examination on you, to confirm that you do not have any conditions that could interfere with your surgery or the outcomes. He will then arrange for you to have a CT or MRI scan of your hip at least 6 weeks prior to your surgery date. This gives the engineers enough time to create the 3D model of your hip for Dr Singh to check over and for your personalised surgical instruments to be manufactured.
Dr Singh also recommends that you meet with a physiotherapist at least once (preferably twice) before your procedure who will teach you exercises that can greatly improve and hasten your recovery post-surgery.
Total hip replacement surgery
Total hip replacement surgery (also called total hip arthroplasty) involves replacing the top (proximal) part of your thigh (femur) bone, and the inside part of the hip socket (acetabulum). These parts of the bones in the hip joint are covered in articular cartilage which can wear out as you get older, and it is this degenerative process which is known as osteoarthritis.
In total hip replacement surgery, these damaged hip joint surfaces are replaced with highly resistant metallic and ceramic components called; the femoral stem (Titanium- Niobium alloy), a femoral head (BIOLOX delta Ceramic) and a Cup (pure titanium alloy). Inside the metal cup, a liner (highly crosslinked Polyethylene or BIOLOX delta Ceramic) is inserted, which replaces the cartilage and synovial fluid function, allowing your pelvis bones to slide smoothly on each other again, and ultimately eliminate your pain and stiffness.
YOUR TOTAL HIP REPLACEMENT AT MIDWEST ORTHOPAEDICS
1.HIP IMAGING
At least 6 weeks prior to your surgery date, Dr Singh will arrange for you to have a CT/MRI scan of your operative hip.


2. REPLICATION OF YOUR HIP
Using the images from your CT scan, engineers create a 3D model of your hip
3. ANALYSIS AND PLANNING
Dr Singh closely analyses your 3D hip model and then makes any necessary adjustments to your surgical plan so that the final position of your hip implants can be precisely matched to your specific anatomy.

4. YOUR SURGICAL INSTRUMENTS (MyHip) ARE PRODUCED
Your surgical cutting guides and the 3D model of your hip are manufactured, sterilised, and sent from o/s, across to the hospital in time for your procedure.
5. INTRAOPERATIVE VERIFICATION
Dr Singh utilises software in the operating room that assists him during the intra-operative assessment of your leg length, offset and cup angles values to achieve the most accurate implant sizing and position for you.

Suitable candidates for a hip replacement
People with hip pain (osteoarthritis) that is no longer being relieved by their nonsurgical treatments and the pain is occurring frequently, is interfering with their day-to-day activities, and reducing their overall quality of life, may be considered for total hip replacement surgery.
To diagnose hip joint degeneration, Dr Singh will go through all your medical history, followed by a physical examination. Your medical history is compiled by asking you questions about your hip pain, any medications you may be taking, and prior injury and other bone and joint problems you may have. The physical examination will evaluate your range of motion and Dr Singh will observe how you walk, sit, bend, and move which all assist with your assessment and diagnosis.
Further testing may be required including x-ray’s, blood tests, or an MRI and your hip surgery is recommended only after careful diagnosis of a hip problem, including your degree of pain and lack of mobility.
Benefits of a hip replacement
A successful hip replacement procedure (which occurs in 95% of patients), provides pain relief and restores mobility, allowing your hip to move freely again. Following a total hip replacement procedure with Dr Singh, your new hip should be stable and permit activities such as swimming, cycling, and walking and sports such as fishing, bowls, golf, and doubles tennis to be played again.
- Reduction in hip pain
Your pain will be rapidly and dramatically reduced, and usually eliminated - Recovery of mobility
Your hip will function with less effort, almost regaining its original mobility after surgery - Improvement in your quality of life
Your everyday activities should no longer be limited by pain and reduced mobility!
Prosthetic implants used in hip replacement surgery
The prosthetic implants Dr Singh uses in your total hip replacement procedure consist of three different parts: the acetabular component, the femoral component, and the articular interface.
- Acetabular Component: In the Acetabular component, cartilage and bone are removed and a cup (made from titanium alloy with a highly porous plasma spray coating to facilitate bone in growth and stability), and liner (highly crosslinked Polyethylene or BIOLOX delta Ceramic), are placed into your acetabulum (hip socket). The liner is inserted into the cup and locks securely in place and provides a smooth, gliding inner surface that will allow you to move easily again, and without pain like a hip that is healthy.
- Femoral Component: This is the prosthetic component that fits in your thigh bone (femur). To implant the femoral component, Dr Singh removes the worn proximal (top) part of the femur bone and sizes your femur with a range of instrumented broaches to receive the femoral stem (made of Titanium- Niobium alloy), and the femoral head (made of BIOLOX delta Ceramic). There are a wide range of femoral stem implant options and head sizes to allow for the accurate reconstruction of your hip joint (restoring your native soft tissue laxity (offset) and leg length).
- The Articular Interfaces: There are two articular interfaces (involving the liner and femoral head) that Dr Singh may use in your procedure, depending on your individual circumstances:
Ceramic on Poly – This is generally used when Dr Singh requires the use of additional stability in the form of a lip built into the liner, and you have a smaller sized acetabular socket and femoral head.
or
Ceramic on Ceramic – This combination is used when your acetabular socket is of a larger size and can receive a larger size femoral head. It is particularly useful to reduce volumetric wear rates of the interfaces and provide you with optimal stability with a good range of motion.
*Dr Singh does not use the metal-on-metal bearing surface combination in any of his hip replacement surgical procedures, nor has he ever used them because of the metal debris they can develop.
Technology in hip replacement surgery
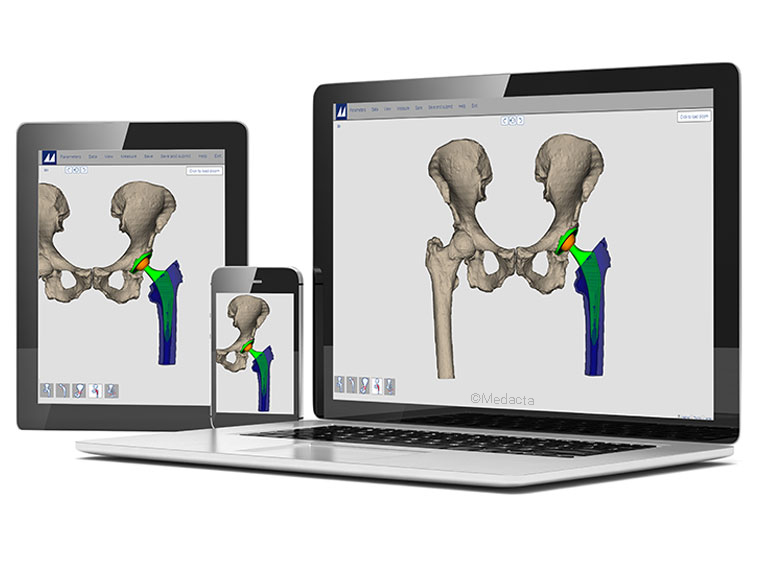
Dr Singh usually utilises the MyHip advanced system in his total hip replacement procedures which is specifically designed to assist him with your implant selection and positioning. This system addresses the challenges in surgery and streamlines the pathway to a carefully planned hip replacement procedure, though 3D preoperative planning and 3D printed patient-specific guides.
The 3D preoperative plan is created from your CT/MRI scans, taken 6 weeks prior to surgery, and are based on Dr Singh’s preferences and your individual anatomy. The plan is submitted to Dr Singh for approval through an interactive website where he can modify your implant type, size and position. Once Dr Singh has approved your 3D preoperative plan, the implant manufacturer then produces your 3D printed guides (surgical instruments) using in-house laser sintering technology. Once produced, your surgical guides are then sterilised and sent across to the hospital along with the 3D model of your hip in time for your procedure.
To further support your surgical outcomes and potentially reduce surgical outliers, Dr Singh also utilises an advanced intra-operative verification platform in the operating room during your procedure. This technology further assists him during the intra-operative assessment of your leg length, offset and cup angle values and enables,’ real-time’ and accurate numerical evaluation of the parameters crucial for the success of your surgery.
Dr Singh recognises that everyone moves differently and so this technology is an important consideration when performing hip replacement surgery.
Hip replacement surgical approaches
There are multiple surgical approaches that can be used to perform a total hip replacement surgical procedure including, the Posterior (back) approach, Lateral (side)approach, Antero-Lateral (back & side) approach, or the Anterior (front) approach.
Some approaches can be more muscle sparing than others which may lead to a quicker recovery however, the most important aspect of any hip surgery is to ensure that the prosthesis is implanted correctly and accurately, that the surgery is carried out in an efficient manner, minimising blood loss and reducing anaesthetic time and that the risk of complications are kept to a minimum.
The total hip replacement surgical procedure
Your total hip replacement procedure starts off with you being wheeled into the operating bay and meeting with a member of the anaesthesia team. The most common types of anaesthesia used in a total hip replacement are general anaesthesia (you are put to sleep) or spinal, and/or regional nerve block anaesthesia (you are awake, but your body is numb from the waist down).
The anaesthetist, with your input, will determine which type of anaesthesia will be best for you.
After the anaesthetist has administered your anaesthetic and the nerves that supply your tummy, hips, bottom, and legs have been numbed, Dr Singh will make an incision to allow access to your hip joint. Your worn hip socket (acetabulum) is then reamed in the shape of a sphere and a new titanium shell (cup) is pressed in place. Inside the metal cup, a liner is inserted, and your old ball (femoral head) is removed. The top of the thigh bone (femur) is reshaped to accept the thigh part of the hip replacement, (femoral stem) which is then pressed in place. A ceramic ball (head) is placed on the top, and this is then placed inside the liner completing your new hip. Dr Singh utilises advanced software in the operating room throughout the surgical process which assists him with the intra-operative assessment of your leg length, offset and cup angle values and enables,’ real-time’ and accurate numerical evaluation of parameters.
At the end of the procedure and prior to closing the skin, Dr Singh may inject local anaesthetic all around your hip to help manage your pain.
The surgical procedure usually takes between 1 to 2 hours in total.
Managing you total hip replacement surgical pain
To minimise total hip replacement surgery pain, Dr Singh adopts a tri-pathway pain management approach. The first pathway involves the use of an effective local anaesthetic block at the time of your operation which numbs all the parts which have been operated on and which may generate pain. The second pathway utilises oral pain medications which Dr Singh’s team will prescribe for you. Injections are also available if required and, the third pain management pathway incorporates a quick visit at Dr Singh’s rooms for your wound check to further minimise any post operative pain.
Hip replacement surgery recovery timelines
Immediately after total hip replacement surgery, you will be wheeled into a recovery room on your ward bed and given oxygen to help you breath. Leads will be on your chest to monitor your heart rate, and an intravenous line (drip) will be in your arm which dispenses fluid and paracetamol for the first 24-36 hours following your procedure and there will be a dressing over your incision.
When you wake up in the recovery ward, you may feel a bit groggy. Dr Singh and the hospital team will monitor you, checking your blood pressure, temperature, and pulse. Post-operative x-rays will be performed in recovery so that Dr Singh can check the position of your prosthesis. After 45 minutes – 1 hour, you will be transferred back to your room on the ward.
The nursing team at the hospital will help you perform your normal day to day activities as required. The hospital physiotherapists will also help you to achieve independence with the following post-surgery goals:
- Lifting your leg in and out of bed (using a small device)
- Walking with a frame
- Walking with crutches or a walking stick on a level surface
- Walking up and down stairs
- Getting in and out of a chair
- Going to the bathroom
Your hospital stay following total hip replacement surgery is usually 3 nights, however, may be longer based on your individual situation. Dr Singh takes into consideration your age, general health, whether you have help at home, if your home has a lot of steps among other factors when determining your required stay in the hospital.
In the first week following surgery, you may experience:
SWELLING– From your thigh down into your foot is common. Swelling may increase for the first few days after surgery and will gradually lessen although some swelling can still be present for 12 months or so after surgery.
BRUISING – Bruising is common and can usually be found anywhere on your thigh and down into your foot. At times the bruising can be quite dramatic, but it will resolve. Bruising is the result of some residual bleeding making its way to the surface or, it can also come about from the blood thinning tablets you will be taking.
BLISTERING – In some patients, blisters will develop near your incision. The blistering is usually due to surface fluid, and although they may look alarming, they are usually of no consequence. Blisters can be caused by the bandages rubbing on your skin or from tissue swelling. They may burst and leak fluid and can sometimes be large and alarming, but they are harmless, and will always resolve.
MUSCLE SORNESS – During surgery, some stretching and pulling on your muscles occurs. Your muscles can feel stiff and sore to touch with pain like a corked thigh. Walking and stretching can usually help alleviate this.
INCISION WARMTH – For some patients, the operated hip may radiate heat and feel very warm. This is because, part of the body’s natural healing process is to supply more blood to areas in the body that have been wounded, and it is the extra blood around the incision which creates the warm feeling.
For the first 2 weeks after surgery, your activity level is usually limited however you will be able to walk independently, use the bathroom and perform normal daily activities.
After 2 weeks, you will be able to engage in moderate activities, such as driving a car and climbing stairs.
Within 6 weeks, you should be able to resume most of your normal activities.
Follow-up appointments with Dr Singh following total hip replacement surgery are 1 month, 3 months then, 12 months post-surgery. The Arthroplasty Society of Australia recommends that all total hip replacement patients are reviewed again every three years so, you will be contacted for this appointment around that time also.
Precautions following hip replacement surgery
Following a total hip replacement surgical procedure, the muscles and soft tissues around the hip are often weaker and therefore unable to stabilise the hip as per usual. Because of this, the following hip precautions for 6 weeks, post-operatively should be strictly followed:
- No bending at the hip past 90 degrees. This includes reaching towards the ground, picking things up, or sitting on low surfaces. (Grabbers are helpful as are shoehorns)
- Avoid the combined movement of bending your hip whilst turning your foot in
- No crossing your legs whilst sitting, lying, or standing
- Do not excessively rotate your legs either inwards or outwards
- Do not lift your leg straight up in the air
- Do not force your leg backwards
- No hopping, skipping, or jumping on either or both legs
- DO sleep with a pillow between your legs
- DO apply Vitamin E or moisturising cream on the wound once it has healed
Potential hip replacement surgical risks
The majority, (95%) of total hip replacements are performed without complication, resulting in a painless hip which is stable, and should last at least 20-30 years using modern day implants.
As with all surgeries however, there are certain risks and potential complications. The following is a list of possible complications, and the measures Midwest Orthopaedics uses to mitigate them from occurring:
Blood clots: Clots (deep venous thrombosis or DVT) can occur in the veins of the legs after any surgery. Occasionally these clots travel to the lungs causing a clot in the lung (pulmonary embolus or PE). A pulmonary embolus has the potential to cause death so, if you develop pain or swelling in your calf post-surgery or find yourself suddenly short of breath, please contact Midwest Orthopaedics, the hospital, or your local GP immediately.
To reduce the risks of clots forming, Dr Singh will prescribe aspirin to thin your blood and he uses special compression sleeves during and after your operation. The Midwest Orthopaedics team will also spend time educating you on calf muscle exercises to be performed after surgery and ensure the hospital team get you up and mobile as quickly as possible after surgery.
Infection: This is a very serious complication which occurs in approximately 1% of cases.
Although uncommon, the Midwest Orthopaedics team take the following precautions to further minimise this risk:
- prior to surgery, your skin is tested to ensure resistant organisms are not present
- your limb is prepared with antiseptic on the ward prior to surgery
- intravenous antibiotics are used at the time of surgery
- the surgical team are required to wear special, self-enclosed theatre gowns
- any infection that develops after surgery is treated immediately
Delayed infection has been reported years after joint replacement and appears to be related to the ability of the implants, in general, to harbor bacteria transported by the blood stream from other sites of the body. Bladder or kidney infections can be a source, but dental abscesses, infected ingrown toenails, or skin infections may also be a significant danger to a joint implant. If dental surgery, bladder surgery, bowel surgery or rectal surgery is planned, the surgeon or dentist should be informed that you have had a joint replacement.
If an infection does occur, it is important to seek treatment immediately as it is often possible to save the prosthesis if treated early enough. If this is not possible, then it may be necessary to remove the prosthesis and give antibiotics through a drip for a six-week period.
A new prosthesis can usually then be re-implanted once the infection has resolved.
Fracture: Although rare, it is possible for the top part of the thigh bone (femur) to crack during insertion of the femoral stem prosthesis. Dr Singh avoids this risk by taking appropriate care during insertion and using a hip replacement system with many size options.
Prosthesis loosening: A small percentage of patients require revision surgery because of excessive wear of the ball and socket joint or loosening of the prosthesis. This may cause pain and a limp, and the diagnosis can be confirmed with x-rays. Excessive wear of the ball and socket joint is one of the most common reasons why revision hip surgery is performed.
Dr Singh reduces the risk of this occurring by using a ceramic femoral ball (head) which gives a very low wear rate. He also avoids the use of cement by using a prosthesis which has a ‘bone like’ coating allowing the patient’s bone to grow directly onto it.
Implant malposition: Despite the best intentions and effort, it is possible for a prosthesis to be inserted at a slight angle or rotated. To avoid this risk, Dr Singh utilises advanced software in the operating room during your procedure which assists him during the intra-operative assessment of your leg length, offset and cup angle values.
Hip dislocation: Sometimes, the ball and socket joint can dislocate following total hip replacement surgery which would cause acute pain and the inability to walk. The hip can usually be put back in place by manipulation without the need for open surgery and dislocation is more common in the first few months postoperatively.
Dr Singh reduces your risk of dislocation following total hip replacement surgery by:
- preserving as much of the hip’s normal muscles and tendons
- correct positioning of the hip prosthesis
- using a femoral stem with variable offset to allow better muscle tension
- educating his patients on correct positioning of the leg
- maximizing the strength of muscles around the hip with exercises before and after the surgery
- by using patient matched instrumentation and technology during surgery
Leg length discrepancies: Most patients are shorter in the arthritic leg before their surgery, and this is corrected during the procedure. Patients may feel tilted for a couple of months until they get used to the normal position of their hip. If the other hip is arthritic or, if they have a curve in their back (scoliosis) this feeling will continue. It is rare for the difference to be more than 1cm however, on occasions, a small shoe raise adjustment may be required even after surgery.
Dr Singh reduces the risk of you developing a large difference in leg length by utilising technology in surgery, measuring the changes in leg length during the operation, and by using a prosthesis with variable ‘offset’ as well as length.
Allergies to metal: Metal allergies, particularly nickel, can occur in some people. The prostheses Dr Singh uses are made of titanium, ceramic, and polyethylene. They do not contain nickel so should not cause an allergy.
Damage to nerves and arteries: Important nerves and arteries lie close to the hip joint, and it is possible, although very rare, for these to be injured during total hip replacement surgery. Should this occur, further surgery may be necessary to repair the nerve or artery and reduce the chance of permanent damage occurring.
With modern prosthetics, advanced technology and meticulous care, injuries to other structures around the hip are now extremely rare.
The patients general and mental health: As with all surgeries, patients can develop problems such as a heart attack or stroke during or after an anaesthetic. This is often related to health problems present before the surgery though and is why Dr Singh arranges a specialist physician review prior to your procedure.
Discovering any potential problems before surgery drastically reduces the risk of any of these complications from occurring.
Total hip replacement surgery | estimate of fees
Typically, costs associated with total hip replacement surgery as a privately insured patient at Midwest orthopaedics include your initial consultation fee, review consultation fee & Dr Singh’s surgical fees. Other related charges include the Anaesthetist, the hospital fees, implants/prosthesis and any in-patient pathology and radiology charges if x-rays or scans were required:
- Initial consultation fee – $76.80 back from Medicare
- Review consultation fee – $38.60 back from Medicare
- Surgical Fees – For privately insured patients, Dr Singh’s fees are typically a proportion of the AMA Fee or a “Known Gap” Fee. Please check with your health fund to ensure you have appropriate cover.
- Anaesthetist’s fees – The Anaesthetist s fees will be given to you by the hospital. Your anaesthetist will contact you prior to surgery and obtain informed financial consent.
- Hospital fees – If you have private health insurance this is confined to your excess, but certain orthopaedic procedures are excluded from some policies and therefore should be checked prior to booking in.
- Pathology and radiology – These are blood tests and imaging taken during your inpatient stay that may also incur added costs.
- Implants and prosthesis – Most of these are covered by your insurance company, but once again it is important to check with your health fund prior to the surgery.
Your level of healthcare and your provider greatly influence your out-of-pocket expenses, so we recommend that you check with your health fund prior to booking in for surgery.
Self-Insured Patients
An increasing number of people without private health insurance are choosing to “Self-Insure” or pay for their own surgery. This is because, even though Dr Singh operates in the public sector at Geraldton Regional Hospital, the waiting list to even meet with him can be long (too long), followed by even longer waiting lists for their operation.
All the private hospital fees associated with your surgery are however an out-of-pocket expense. Our team can assist you in obtaining an estimate of costs before proceeding.
Discover more about hips
 Christmas Operating Hours
Christmas Operating Hours 










